Algorithms are the driving force in translating clinical data into actionable insights that are useful and meaningful for the patient and his doctor. But it’s hard to write an article on something as ‘invisible’ and abstract as algorithms and to convince the reader of the immense possibilities of this building block for medical devices, wearables and other healthcare-related products (such as drug-device combinations).
That’s why imec’s principal scientists, Willemijn Groenendaal and Evelien Hermeling, chose to illustrate imec’s approach in this field with some concrete studies on specific diseases and therapies. Let’s dive into 4 pioneering studies on cardiac monitoring, cardiac rehabilitation, stress management and decongestion therapy illustrating the cornerstones of imec’s approach:
- Algorithm-assisted labelling of raw data by identifying so-called fiducials (e.g. the R-peak in ECG data)
- Identification of new biomarkers
- Translating the data into actionable insights
- Assessing the quality of the signals, the biomarkers and the insights
- Partnering with hospitals to perform studies with patients to evaluate new (sensing) technologies and algorithms
1. Algorithm-assisted labelling of time series
A new tool
The first step in moving from data to insights is often detecting so-called fiducial points in the data, such as the R-peak in an electrocardiogram signal. The location of these R-peaks can be used to e.g. calculate the heart rate of a patient. Recently, imec developed a key building block that forms the base for its research in this area.
Evelien Hermeling: “Imec developed a unique and user-friendly platform for analysis and labelling of medical signals. It’s a new tool, designed in Python, that will make life much easier when it comes to developing, training and validating new algorithms.”
“The core of the platform is a graphical user interface that facilitates three main types of manual annotations: (1) Time and/or amplitude fiducials, e.g. R-peaks of ECG; (2) Events with duration, e.g. arrhythmic episodes; and (3) Signal quality, e.g., data parts corrupted by motion artefacts."
"All annotations can be attributed to the same signal simultaneously in an ergonomic and user-friendly manner. The platform allows to plug-in existing algorithms and to manually correct them where needed. It enables fast annotation of several signal modalities (cardiac, respiratory and more) and can be used to further improve algorithms and importantly validate algorithms.”


With imec’s user-friendly platform for analysis and labelling of medical signals, it becomes easier to develop, train and validate new algorithms for many health applications. In these 2 graphs, a PPG signal is shown, labelled in terms of activities, motion artefacts and other regions of interest (top) and in terms of signal quality (bottom) (blue, green and red colour bars stand for different signal quality levels assigned to 10 s segments).
Study illustration: artificial intelligence labels ECG data in a cardiac monitoring device
For the diagnosis or follow-up of heart conditions, a continuous monitoring of electrocardiogram (ECG), while the patient performs his/her daily activities, is beneficial. In ECG data, it is important to detect and label the R-peak, to calculate from this the heart rate and other important cardiac parameters. It is also an important metric to diagnose arrythmia.
Willemijn Groenendaal: “Imec has published several papers on ECG beat detectors, algorithms that can detect the R-peak and the 5 distinct (P-Q-R-S-T) waves of the ECG complex, as well as the time in between beats. Part of this work was done together with the hospital ’Ziekenhuis Oost-Limburg’ (a supra-regional hospital in the Belgian province of Limburg)."
"The research focuses on making these beat detectors low-power, fast (to work in real-time), accurate and intelligent. All these characteristics are important if you want to embed the algorithm in a small wearable device. ‘Intelligent’ refers to the use of deep learning and unsupervised-learning techniques in the beat detector.”
Evelien Hermeling: “Adding intelligence to the wearable device, so-called edge computing, has many advantages. First of all, it circumvents privacy issues which are a problem in today’s wearables that rely on cloud services for data analysis. Further, it allows for a more scalable solution since less data need to be transferred from the wearable to the cloud. And finally, edge computing is a more energy-efficient approach as compared to cloud computing.
2. Identifying new biomarkers
After annotating important fiducials in the data stream, algorithms are needed to identify biomarkers that give information on one or several physiological systems in the body. For example, heart rate is a biomarker, extracted from the ECG signal (that in a first step has automatically been labelled with the fiducials P-Q-R-S-T), that gives information about the health and physical condition of the patient. Another example of biomarkers are inspiratory time and volume, or respiratory frequency, for patients with a chronic lung disease.
Study illustration: bio-impedance of the chest as a biomarker for fluid changes in the body during decongestion therapy
Heart failure (HF) is a major public health problem worldwide and is characterized by frequent (re)hospitalizations that are mainly caused by congestion (i.e. water and sodium retention in the body).
Therapeutic strategies to manage congestion include diuretics, vasodilators, ultrafiltration, etc. The problem is that for each patient, the appropriate decongestion strategy must be found. Could wearables and algorithms monitor the efficacy of the treatment to support a personalized therapy setup?
Researchers monitored 36 patients during their decongestion therapy in the hospital ‘Ziekenhuis Oost-Limburg’ *. A wearable device on their chest monitored the bioimpedance. It could be concluded that bioimpedance-based monitoring can be used to assess changes in a patient’s fluid status (i.e., the efficacy of decongestion therapy during hospitalization). The bio-impedance biomarker could even be used to gain insights on the therapy: patients with an increase in thoracic impedance during initial treatment tended to have a better clinical outcome than patients without an increase in thoracic impedance. This clinical outcome was recorded 30 days and 1 year after the hospitalization.
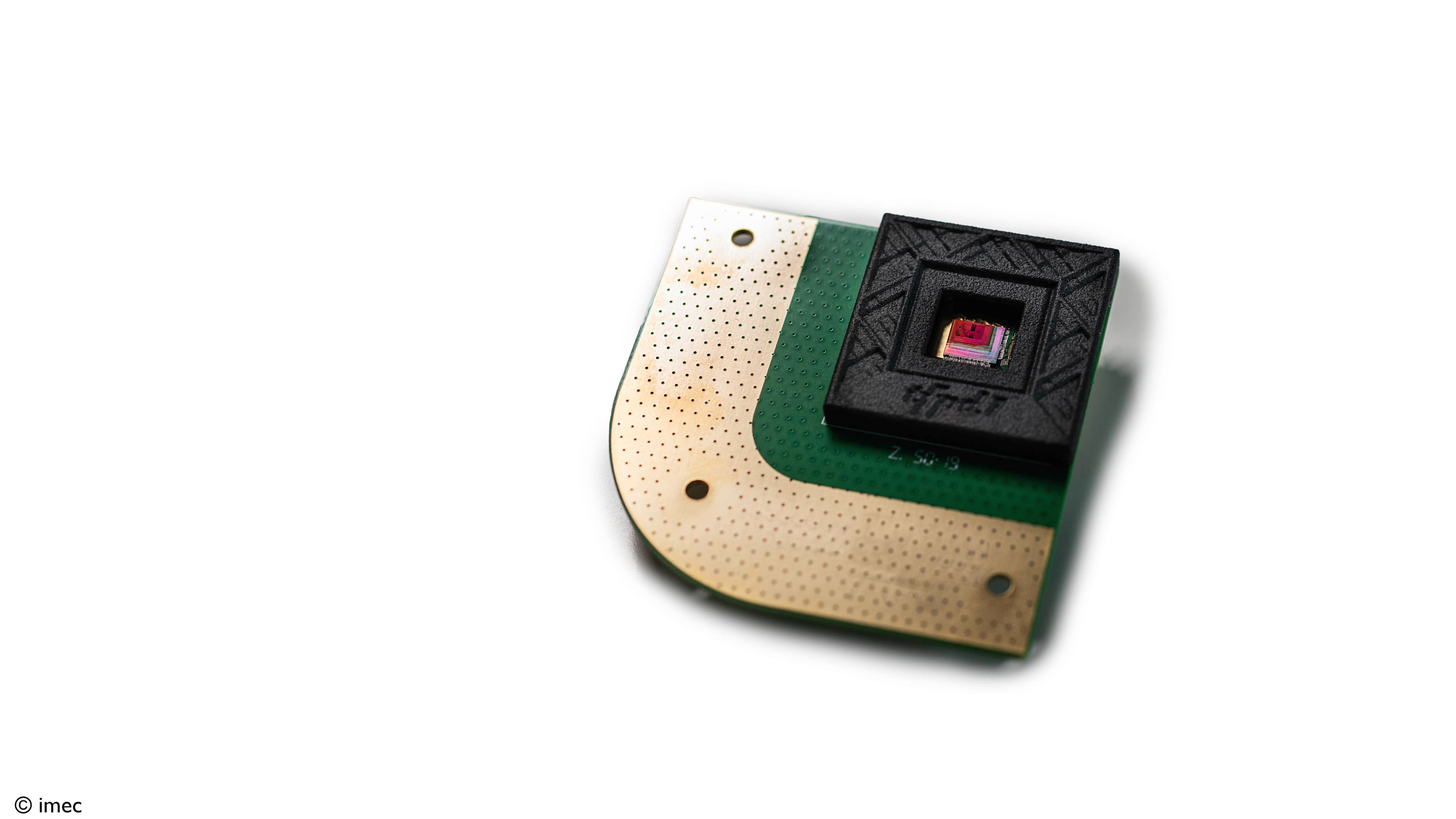
Willemijn Groenendaal: “In this study on decongestion, as in many of our studies, we use our own chips and wearable monitoring devices for ECG, skin temperature, bio-impedance etc. We develop both the hard- and the software and it is this integrated approach that has led to a unique set of expertise which are key to develop truly innovative health solutions. Especially when in the future more intelligence will be added to the wearable, insertable or implantable device itself, an intense collaboration between hard-, software and application experts is mandatory.”
Future outlook: more complex biomarkers
Evelien Hermeling: “The development of novel biomarkers is something we strongly focus on. Examples of ‘standard’ biomarkers are heart rate, heart rate variability, skin temperature etc. But what if we could devise biomarkers for more complex things such as inflammation, oxidative stress or endothelial dysfunction and measure this in a non-invasive way? The latter is linked to the endothelium, a thin membrane at the inside of the heart and blood vessels. When it’s not functioning well, the arteries cannot fully dilate, and problems arise. These biomarkers are important in predicting stroke, heart attacks, and other cardiovascular conditions.”
“To be able to measure such parameters in a non-invasive way, we would need to collect data with a wearable (e.g. a patch) and use algorithms to calculate from this certain biomarkers that are a measure for e.g. endothelial dysfunction."
"The first step would be of course to devise this new biomarker for endothelial dysfunction through data collection in clinical settings, together with physicians and other application-knowledge experts such as medical device companies. From this, scientific publications are prepared to convince the medical community about the value of the new biomarker and about the reliability of the measurement with wearables and algorithms. The next step, and the ultimate goal, is to then further develop the solution to be used in an ambulatory and home setting.”

Multimodal monitoring of heart-failure patients enables comprehensive insights in patient wellbeing and disease status.
3. Translating the data into actionable insights
A third category of algorithms (besides the ones for identifying fiducials and calculating biomarkers) is developed to gain actionable insights out of the data.
Willemijn Groenendaal: “At this level, we combine data from multiple biomarkers, physiological systems and body-subsystems (heart, respiration, exercise, ...) to make decisions on the specific disease. In a study on COPD (Chronic Obstructive Pulmonary Disease) patients that we did for example, novel combinations of bioimpedance and myography parameters showed differences between patients with different disease severity levels. These novel indices could one day be used to monitor, in a continuous way, the progress of the disease, at the patient’s home. Of course, further studies and developments are needed.”
Study illustration: algorithms predict the outcome of cardiac rehabilitation and pave the way to a patient-tailored approach
For people who have experienced a heart attack, heart failure, angioplasty or heart surgery, a cardiac rehabilitation program is often set up to improve their cardiac health. One of the key components of this therapy is exercise counselling and training.
Not all patients respond in a similar way to cardiac rehabilitation (CR) and little is known about the mechanisms causing the large variability among patients. Could algorithms assist physicians in gaining more insights into CR, predicting its outcome for specific patients, and working out a patient-tailored approach?
To investigate this, researchers collected data from 129 patients, doing a CR program in the hospital ‘Ziekenhuis Oost-Limburg’ *. The patients wore imec’s wearable electrocardiogram (ECG) prototype device while performing five 6-minute walking tests at regular intervals during their 15-week program.
Based on the ECG data, parameters such as resting heart rate, peak heart rate, recovery heart rate etc. were calculated. It then was investigated if there was a difference in cardiac response between patients that showed a clear improvement in functional capacity (the high-response group) and patients that only showed a minor improvement (the low-response group) following CR therapy.
Willemijn Groenendaal: “In this study, we defined new digital biomarkers: the shape and the steepness of the curve that depicts the heart rate during the 6-minute walking tests. These biomarkers allow for more in-depth insights into the cardiac response of the cardiac patients during standardized activity, and to distinguish the high-response group from the low-response group. Moreover, this differentiation could already be made at the start of therapy (the baseline), where the increase in heart rate during the walking phase was steeper in the low-response group. In this way, the novel biomarkers could be used to predict how a patient will respond to CR therapy, and to personalize treatment strategy.”

Using a wearable ECG device, the heart rate of cardiac-rehabilitation patients was measured during 5 walking sessions. The quadratic polynomial model was used as a fit (the line represents the mean fit and the shadows represent the SD) and the coefficients for the shape and steepness of the curve are proposed as new digital biomarkers to predict the outcome of CR therapy. (copyright: De Cannière et al.).
Willemijn Groenendaal: “You may have noticed that this research is done in close collaboration with a hospital, the ‘Ziekenhuis Oost-Limburg’. Clinical collaborations are a corner stone in every of our studies. Our algorithms must first be validated in a clinical context, with application experts involved, before they can be used in wearables for home monitoring.”
4. Assessing the quality of the data, at all levels
As important as identifying fiducials, defining biomarkers, and gaining insights from the data, is the focus on the quality of all these findings. Imec develops algorithms that indicate the quality of all these levels, which is important information for the physician when devising a strategy for the patient. This quality indication is of uttermost importance for measurements in the home setting, outside the controlled environment of the hospital.
Study illustration: stress monitoring during daily activities
Stress has a negative impact on our health and wellbeing. Studies suggest a correlation between stress and depression, cardiovascular disease, sudden death, and myocardial infarction. Early detection and prevention of stress are therefore of utmost importance.
Algorithms and wearable devices hold the promise to assist in personalized prevention and treatment strategies, taking individual variability in stress parameters into account. Imec did a large-scale study in which 1002 people were monitored for 5 days, during their daily activities. Using wearable devices (measuring ECG, heart rate, skin conductance, skin temperature and movement), smartphones (for contextual information) and smartphone-based questionnaires, the largest dataset ever reported on ambulatory stress monitoring, was collected.
Algorithms and machine learning were used to analyze the data and it revealed significant differences in ECG parameters, skin temperature, and skin conductance for different stress levels. Also, it was concluded that physiological responses to stress strongly differ among people: some show a small and others a large dynamic range of the physiological features. In other words: people differ in the magnitude and type of their physiological stress response. The study found that the group with a more blunted physiological stress-reactivity (small dynamic range) tend to report a less healthy lifestyle and higher depression, anxiety and stress scores than the more responsive group (large dynamic range).
Evelien Hermeling: “This study is a great example of how wearable monitoring, in real-life conditions, can lead to new insights in diseases and mental conditions. This in turn forms the base for new therapy strategies, potentially assisted by wearable technology.”
Willemijn Groenendaal: “One of our focus points, also in this study, is to take into account the quality of the signals. Within imec, we believe quality indicators should be used at all levels (signal-level; biomarker-level; insight-level) to help interpret the data in a correct way. Also, we try to use different methods to measure one parameter and use signal fusion to improve the reliability of the measurements.”
The next big thing in patient-centric healthcare: a holistic approach
Evelien Hermeling: “Today, the focus is often on one health parameter and how to optimize this. Think for example of blood pressure. The cardiologist will monitor his patient with a wearable or hospital device, adjust the medications, maybe even use a drug-device combination to perfectly balance and personalize the drug dosage. However, the ideal blood pressure may not always lead to the optimal overall health status. Indeed, blood pressure medication can depress heart rate, and this will make it more difficult to stay active. Wouldn’t it be better if a wearable could measure different parameters, and algorithms could assist in finding the perfect balance to achieve a good overall health? At imec, we believe that such a holistic approach (the optimization of a whole group of biomarkers) will be at the base of a patient-centric healthcare.”

A holistic approach aims at measuring different parameters, whereafter algorithms assist in finding the perfect balance to achieve a good overall health.
Conclusion
Although imec is best known for its semiconductor technology, an enormous amount of expertise in algorithms, AI and machine learning is also present. In this article, we demonstrated this for the domain of healthcare through some impressive studies on stress management, cardiac monitoring, cardiac rehabilitation and decongestion therapy.
Imec’s focus is on:
- A strong validation of the algorithms by using large and various datasets
- Collaboration with hospitals for the clinical validation of the algorithms
- Quality assessment at all levels
- Explainable AI, because this is the way to go for clinical acceptance
- An integrated approach, aligning chip design, system build-up and software
- A holistic approach, optimizing different biomarkers at the same time
Imec collaborates with clinical partners, medical device companies and pharmaceutical businesses to bring these results into products that will change the life of many patients.
* as part of a PhD project of the Mobile Health Unit, a collaboration between Hasselt University, Jessa Hospital and Ziekenhuis Oost-Limburg focused on academic clinical research in mobile health (Limburg Clinical Research Center).
Want to know more?
- Discuss your idea with Zohaib Gulzar, our business development manager.
- Discover the different ways of working with us.
- Get a nice overview of imec’s connected health solutions.
- Subscribe to our regular updates on the connected health research
- Learn more about imec.
- Read more detailed info in these scientific papers that where mentioned in this article:
- Read the paper ‘Real time electrocardiogram annotation with a long short term memory neural network’ from Corradi et al.
- Read the paper ‘Using biosensors and digital biomarkers to assess response to cardiac rehabilitation: observational study’ from De Cannière et al.
- Read the paper ‘Wearable monitoring and interpretable machine learning can objectively track progression in patients during cardiac rehabilitation’ from De Cannière et al.
- Read the paper “Large-scale wearable data reveal digital phenotypes for daily-life stress detection” from Smets et al.
- Read the paper “The added value of in-hospital tracking of the efficacy of decongestion therapy and prognostic value of a wearable thoracic impedance sensor in acutely decompensated heart failure with volume overload: prospective cohort study” from Smeets et al.
- Request the paper “Platform for analysis and labelling of medical signals” from Fedjajevs et al.

Willemijn Groenendaal is a principal scientist at imec, where she leads research activities with a focus on wearable monitoring and algorithms in the clinical domain. She is involved in studies with patients suffering from COPD (Chronic Obstructive Pulmonary Disease), sleep apnea, and heart failure. These studies are done in close collaboration with hospitals.
Willemijn Groenendaal received her master’s and Ph.D. degrees from the Eindhoven University of Technology, Eindhoven, The Netherlands, in 2006 and 2011, respectively. She has been a Postdoctoral Associate with the Weill Cornell Medical College, New York, NY, USA.

Evelien Hermeling received her PhD degree in 2009 at the Maastricht University, the Netherlands. After a few years of post-doc at Maastricht University, she started as senior researcher at imec in 2015 and became principal scientist in 2019. Her drive is to bridge the gap between hardware-, software- and biomedical engineers and the medical doctors. She is leading the competence team biomedical algorithms and models within imec-Netherlands.
Published on:
2 November 2020