We spoke with Sabine Van Huffel, KU Leuven professor and head of the BioMED team in the electrical engineering department at the faculty of engineering. BioMED is also an imec research group involved principally in making wearables smarter based on unique mathematical models. These models, for example, enable to identify and filter out artifacts in images and to combine (and synchronize!) various measurements for a better diagnosis.
BioMED is working with doctors in the fight against diseases such as rheumatism, heart failure, epilepsy and cancer. It is also working closely with imec to combine the most advanced wearables (from imec) with the best algorithms (from BioMED). A marriage made in heaven!
An engineering team for every doctor
Artificial intelligence (AI) and smart wearables will bring unprecedented advances in medicine. In fact, AI is already helping to make measuring devices in hospitals smarter. For example, these devices can automatically detect epileptic seizures using a cardio-encephalogram (EEG) or identify tumor tissue in images. The algorithms are also very versatile and able to learn new things easily (such as adding a new type of measurement or reading). One important area in which AI is breaking through fast, is radiology. This is because algorithms can handle images easily and learn from the notes made by radiologists.
And thanks to wearables, taking various readings from patients in hospitals can be made more comfortable for them – plus patients can also be monitored at home. The best example of this is in sleep research. At the moment, if you have a sleep disorder, you may have to spend a day in the sleep lab, which is an expensive exercise. But imagine if, instead, you could wear sensors for a month while sleeping in your own bed. Even if these sensors are not as accurate as the ones used in hospitals today, the results would in fact be more reliable because you will be producing readings in a realistic environment and over a longer period of time.
Another good example is monitoring premature babies in a neonatal intensive care unit. For these little tots, not only is it more comfortable to be monitored with wearables (or sensors in the mattress), but it can also be a matter of life or death. Working with the neonatology department at Leuven UZ (University Hospital), BioMED is researching the causes of stress in these babies.
If babies experience stress in the first weeks and months of their development – for example because they have to be hooked up to monitoring equipment and wires – this has an effect on their (brain) development. But by using wearables, they can develop more normally.
Interestingly, wearables will certainly not always take the form of a device that you wear on your body. For instance, sensors can work just as well if they are incorporated into your bed or the seat in your car. When you order a new car, for example, you will be able to add on the ‘health check’ option – just as you do today when you go for heated seats. The same thing with your smartphone. In the old days, these phones were just used for making calls, but now they can do so much more. And in the same way, your car will become more than just a way of getting from A to B!

Imec has developed sensors that can be incorporated into a car seat to monitor your breathing and heart rate. This is just a foretaste of a future in which we might be given a health check while we’re sitting in our car. And sensors built into your mattress at home will measure your sleep quality for the early detection of disorders such as sleep apnea. BioMED is currently developing just such a sleep check with UZ Leuven.
But it will take more than just good hardware and software to make this future come true. Researchers are already seeing that it is no easy matter to convince doctors to work on research into the use of wearables for certain diseases. Why? First and foremost because wearables have to be reliable – and not ‘gadgets’. This means that certification will be very important for making a real breakthrough in this area.
It is also a fact that doctors simply don’t have the time to delve into the mass of data and specific interface of each wearable. Which is why it is important to supplement their training with more technical subjects and also expand their knowledge of AI. For that to happen, though, there will need to be a specialized team of biomedical engineers on hand to assist doctors to deal with this new source of information. After all, a doctor needs to be able to work with the patient and not be weighed down by computer work and huge amounts of data.
So, if we want to be able to use wearables as soon as possible in the day-to-day practices of GPs and specialists, some things have to change. Such as the reimbursement from the patient’s medical fund and the business model to be used. For example, will we buy the wearable from the pharmacy and then throw it away after use? Or is it something we can hire from our health fund? Or will we be given the wearable at the hospital and return it there after use so that a team can disinfect it and reboot it for the next patient?

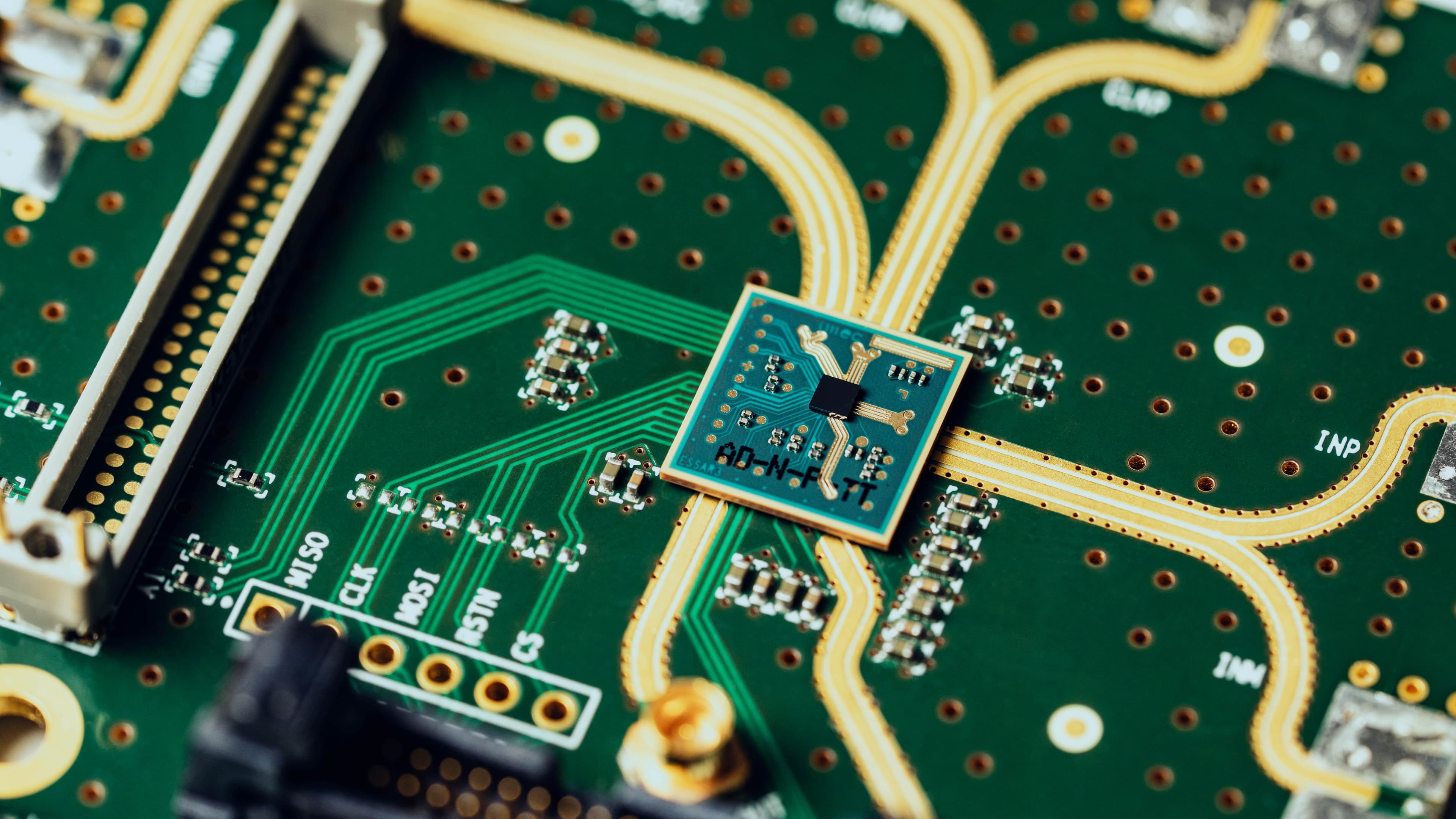
A prototype of a sensor plaster, developed by imec and Holst Centre. This is a good example of what a future with wearables might look like: the user buys a (cheap) plaster at the pharmacy and then throws it away after use – just like a pregnancy test today.
So much for our vision of the future. But where do we stand today? And, more specifically, which of BioMED’s current developments give us a foretaste of how we will use wearables and AI for our health?
Picking up a pen with a sensor
Rheumatism is a common disease whose developments are monitored closely. At the moment, this is done by having the patient do standard exercises at regular intervals with a physical therapist, who fills in a score sheet, stopwatch in hand. What if...
You no longer had to do these exercises, but instead wore a wearable round your upper arm that would recognize when you are putting your socks on, going upstairs, picking something up – and so on.
After all, these are also the actions that are simulated in exercises with the physical therapist. Working with BioMED, the rheumatology department at UZ Leuven has developed a system that consists of a sensor bracelet with an accelerometer which, thanks to BioMED’s ingenious mathematical models, recognizes specific actions in the day-to-day life of the patient. It also measures the time it takes the patient to do something, translating this to a score, just as they do at the moment at the hospital.
The wearable is now being expanded to include heart activity measurements (ECG) so that actions can be recognized even better. The advantage for the patient is that he/she doesn’t have to go to the hospital so often. While for the doctor the benefit is that the exercises reflect real life better and not just a specific moment in the doctor’s surgery when the patient is making a special effort. Many other measuring points can also be recorded over a longer time.

Using this simple wearable and applying smart algorithms, rheumatism patients can be monitored at home.
Mathematics helping to remove a tumor
It doesn’t always have to be wearables, though. The same mathematical models that make wearables smarter can also be used to give doctors more information about doing their work correctly. Example: removing a tumor. At the moment, MRI images are produced using a Magnetic Resonance (MR) scanner. The doctor then uses these images to identify the tumor tissue that needs to be cut out.
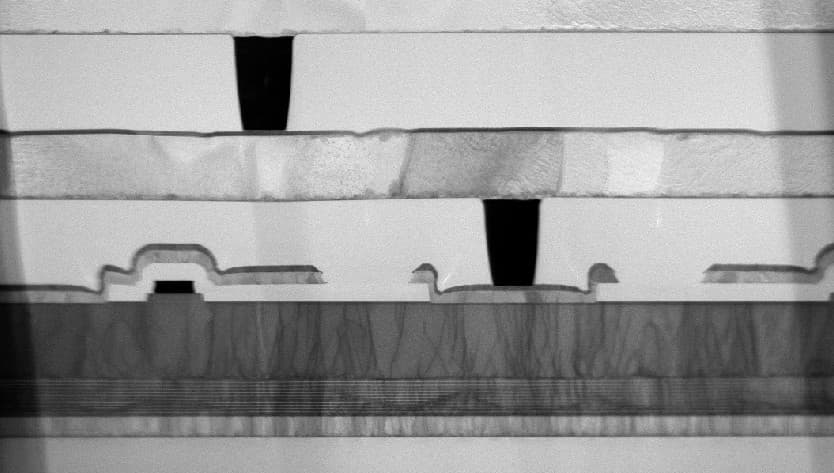
The composition of tumor tissue and healthy tissue is different, which can be seen in the spectrum of a piece of tissue, measured in the same scanner using MR Spectroscopy. When every piece of an MRI image is measured, this is called MRSI (magnetic resonance spectroscopic imaging). If the spectrum of the underlying tissue can be identified for each piece of the MRI image using mathematical models, the doctor is better able to distinguish the healthy tissue from malignant tissue and it is even possible to see gradation differences within the malignancy inside the tumor.
And, because only a specialized spectroscopist can make sense of the spectral images, BioMED has converted the spectral information into ‘fingerprints’ that correspond with the recognizable tissue, while each tissue type is colored on the MRI image. This makes the tumor and its surroundings more straightforward to interpret for radiologists. These algorithms are now ready to be converted into a product that can be used by hospitals and which make MRSI easier to use for radiologists. Working with the radiology department at UZ Leuven and Ghent, the software has already been tested on identifying brain tumors.
Using mathematical models, colors can be added to an MRI image according to the spectrum of the underlying tissue. In fact, this spectrum is a sort of fingerprint for the composition of the tissue and can distinguish in greater detail normal tissue from tumor tissue and necrotic tissue.
Cutting out epilepsy
Some epilepsy patients find medication does not work for them. But, if the siezures are localized (focal epilepsy), then these patients can be helped by the surgical removal of that specific area of the brain.
Typically, patients spend a week in hospital for pre-surgical assessment, during which time they undergo all sorts of tests to localize the particular area of the brain causing the siezures as clearly as possible. EEG readings are taken using electrodes placed on the head, which measure the electrical potential differences (generated by the brain) in high time resolution. Functional MRI (fMRI) also provides important information, while high spatial resolution visualizes the areas of the brain that are active.
But what if you combined EEG and fMRI and took readings together in an MR scanner? Thanks to their complementary resolution properties, this EEG-fMRI combination makes it possible to localize epileptic activity better, both in time and space.
However, the flipside of the coin is that these EEG readings generate additional distortion in an MR scanner, which adversely affects the quality of the readings.
Working with the neurology department at UZ Leuven, BioMED has developed algorithms that enable the ‘epilepsy’ area of the brain to be better localized by combining EEG and fMRI to remove distortion. A software platform is now ready, but needs more multi-centric testing before the software becomes clinically usable.
A ‘hearing aid’ for epilepsy
To help bring a solution to the patient, it is of course always a good thing to have a company on board from the outset of a research project. This was the case in the highly successful imec.icon project, SeizeIT. Working with three companies – UCB, Byteflies and Pilipili, as well as the neurology and pediatric neurology departments at UZ Leuven – BioMED developed a wearable for epilepsy patients. This wearable looks like a hearing aid that is worn behind both ears. By combining the measurements of brain, heart and movement activity, epileptic fits can be detected.
In this instance, these are not the commonly known epileptic seizures in which the arms and legs make uncontrollable movements, but a type of epilepsy where the seizures are much more difficult to identify. To be able to monitor the patient properly and to know whether certain types of medication are working, it is very important to have objective and reliable information about the timing and number of seizures over a specific period. This is now possible with the SeizeIT prototype, which will be developed into a market-ready product as part of a major European follow-up project (supported by EIT Health) .

The ‘hearing aid’ developed as part of the SeizeIT project and which can detect epileptic seizures. This is important for monitoring patients and developing different types of drugs.
Want to know more?
- Are you a company interested in marketing one of these results or taking part in research? If so, please let us know via our contact form.
- If you would like to receive the papers below containing more technical information about the topics discussed in the article, then please let us know via our contact form.
A novel algorithm for the automatic detection of sleep apnea from single-lead ECG
Complexity and nonlinearities in cardiorespiratory signals in sleep and sleep apnea
Accelerometry-Based Activity Recognition and Assessment in Rheumatic and Musculoskeletal Diseases
Interval coded scoring: a toolbox for interpretable scoring systems
Recognition of Physical Activities from a Single Arm-worn Accelerometer: a Multiway Approach
Clinical Decision Support: Interpretability and Applications in Patient Monitoring
Neonatal Seizure Detection Using Deep Convolutional Neural Networks
Quiet Sleep Detection in Preterm Infants using Deep Convolutional Neural Networks
Development of a Neonatal EEG Monitor for Automated Brain Analysis, PhD thesis
A brain-age model for preterm infants based on functional connectivity
Evaluation of a Multichannel Non-Contact ECG System and Signal Quality Algorithms for Sleep Apnea Detection and Monitoring
Probabilistic cardiac and respiratory-based classification of sleep and apneic events in subjects with sleep apnea
Comparison of unsupervised classification methods for brain tumor segmentation using multi-parametric MRI
Semi-automated brain tumor segmentation on multi-parametric MRI using regularized non-negative matrix factorization
Unsupervised and semi-supervised non-negative matrix factorization methods for brain tumor segmentation using multi-parametric MRI data, PhD thesis
Learning from structured EEG and fMRI data supporting the diagnosis of epilepsy, PhD thesis
A prospective fMRI-based technique for localizing the epileptogenic zone in presurgical evaluation of epilepsy
Tensor decompositions and Data Fusion in Epileptic EEG and fMRI Data
Online Automated Seizure Detection In Temporal Lobe Epilepsy Patients Using Single-Lead ECG
Automated Epileptic Seizure Detection Based on Wearable ECG and PPG in a Hospital Environment
Comparison between scalp EEG and behind-the-ear EEG for development of a wearable seizure detection system for patients with focal epilepsy
Epileptic Seizure Detection in a Home Environment, PhD thesis
Adaptive Nocturnal Seizure Detection Using Heart Rate and Low-Complexity Novelty Detection
Online Automated Seizure Detection In Temporal Lobe Epilepsy Patients Using Single-Lead ECG
This article highlights just a few of BioMED’s research topics. For the full story, please visit the BioMED website.

Sabine Van Huffel is Full Professor in Biomedical Data Processing at the Department of Electrical Engineering (ESAT) of the KU Leuven since 2002 and Program Director of the Master of Science in Biomedical Engineering KU Leuven. She received her Master’s degree in Computer Science Engineering, a postgraduate in Biomedical Engineering and a PhD in Electrical Engineering from the KU Leuven, in 1981, 1985 and 1987 respectively. She was a guest professor at Stanford University (USA) in 2000 and at Uppsala University (Sweden) in 2002. She is an IEEE, SIAM and EAMBES founding fellow and member of the Royal Flemish Academy of Belgium for Sciences and the Arts. In April 2013, she received an honorary doctorate from Eindhoven University of Technology (NL). She was appointed Distinguished Professor in 2014.
Sabine Van Huffel is leading a large biomedical data processing research group (25 people), renowned for the development of numerical matrix/tensor-based algorithms, and their applications in biomedical multimodal and multichannel processing and machine learning for improving medical diagnostics. Her expertise techniques include EEG-fMRI, multiparametric MRI, ECG and EEG, focusing on epilepsy and neonatal monitoring.
She has been the supervisor of more than 60 PhD students, mostly all interdisciplinary, as part of joint supervision with her medical colleagues. Sabine is author of more than 400 peer-reviewed international journal papers and more than 400 conference papers. She is holder of an ERC Advanced Grant 339804 BIOTENSORS: “Biomedical Data Fusion using Tensor-based Blind Source Separation”(01-04-2014 till 31-03-2019).
Published on:
7 May 2019